
The Impact of Substance Use and Addiction on Mental Health
Substance use and addiction are complex conditions that can profoundly affect an individual’s mental health, leading to a cascade of negative consequences in various aspects of their life – socially, financially, physically and emotionally. In this first instalment of this series, we’ll explore the definitions and misconceptions surrounding addiction and the prevalence of this issue in Australia.
Defining Drugs and Addiction
Lifeline defines a substance as an illegal drug such as: methamphetamine, heroin and cocaine or non-illegal substances such as: prescription medication, alcohol, glue, petrol, paint and tobacco. Drugs can be used recreationally as well as being used to numb pain both physical and emotional. Some drugs and activities such as gambling are highly addictive which means the user needs to continually consume more of the drug or engage more in the activity to experience the same effect. Often the user will experience cravings and urges to use and experience physical and/or psychological withdrawal when not using.
An addiction is defined by a behaviour where someone is unable to stop using a particular drug or behaviour even if it is causing significant physical and psychological harm. Turning Point a leading drug treatment, advice and research organisation describes addiction as one of the ‘most misunderstood chronic health disorders in Australia’. Current statistics of the prevalence of people experiencing difficulties with gambling, alcohol and other drugs is ‘one in five’ people in Australia. It is seen as one of the major contributors to disease and can affect anyone young and old, from any background, race and ethnicity.
Common Misconceptions About Addiction
Many people misinterpret addiction as a lack of willpower or moral principles. However, it’s a much more complex issue with deep-rooted causes including environmental and genetic factors which predispose imbalances in brain chemistry. St Vincent’s Hospital Melbourne describes addiction as a ‘chronic, relapsing neurobiological disease’. Risk factors that contribute to the progression of abuse and addiction include a lack of family and community connections, economic status, peer pressure, abuse, neglect, early exposure, and mental and physical health problems.
Chinese Medicine Perspective on Addiction
Chinese Medicine offers a unique approach to understanding and treating addiction. For instance, the theory of Yin and Yang is central to Chinese Medicine and describes the ‘dynamic interplay between opposites to achieve homeostasis’. It is the Autonomic Nervous System role to control homeostasis by balancing the sympathetic and parasympathetic nervous system. In yin-yang theory the sympathetic nervous system (SNS) is yang and stimulating such as it; increases heart rate, sweating and breathing. The parasympathetic nervous system (PNS) is yin and depresses the nervous system such as; decreasing heart rate, blood pressure, increasing muscle relaxation and digestion.
The limbic system is the emotional part of the brain and pleasure centre, it encourages reward-seeking and is motivated by the ‘pharmacological effects’ of substances by altering levels of dopamine levels (a yang neurotransmitter). All addictions are yang in nature because they manifest symptoms such as insomnia, anxiety, restlessness, palpitations, nausea, sweating and cravings. The differences in presentation will depend on how much excess heat (yang) the drug causes. Therefore, a fundamental treatment principle in Chinese Medicine would be to clear heat and increase yin that has been consumed by excess yang.
The Role of Acupuncture in Addiction Treatment
Acupuncture, an integral part of Chinese Medicine, has been utilised to treat substance dependence all around the world over the past 30 years. It has gained recognition for its efficacy in addiction treatment, with a focus on Auricular acupuncture to alleviate withdrawal systems, reduce cravings and promote relaxation. In the 1970’s at the Lincoln Hospital in New York, the National Acupuncture Detoxification Association (NADA) devised a standardised 3-to-5-point ear acupuncture technique. The NADA protocol was designed to balance and support the Nervous System by relieving pain, reducing hypertension, anxiety, and depression and facilitating sleep and relaxation. It has been shown to support endorphins, the body’s natural painkillers, by stimulating their release, which helps lessen the physical and psychological suffering related to drug use and addictive behaviours. The NADA protocol is utilised in many withdrawal programs throughout Victoria today.
The 5 points of the NADA Protocol
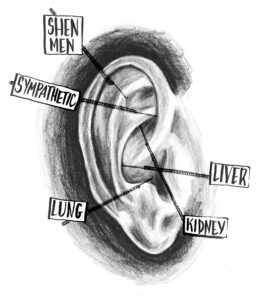
Note: Acupuncture for Community (n.d.).
- Sympathetic – (Spleen & Digestion): Relieves intestine contraction, causing dilation of blood vessels, relieves night sweats. Harmonises the autonomic nervous system balancing both sympathetic and parasympathetic systems. Deeply calming and has a strong analgesic effect.
- Shen Men – (Heart): Calms the mind including pain control, insomnia and harmonises the liver and reduces hypertension.
- Kidney – Relieves lower back pain, relieves urination issues, eye, ear & dental problems.
- Liver – Regulates the free flow of qi, improves eyesight and dizzy spells, fortifies digestion, and relieves chest pain abdominal distension and depression.
- Lung – Controls breathing and respiration, regulates body temperature, alleviates cold and flu symptoms, oedema, night sweats and dysentery.
Treatment with Chinese Medicine
The NADA protocol is primarily used for withdrawal presentations in the acute phase to restore homeostasis and to manage cravings. Your acupuncturist can utilise this protocol in conjunction with an individualised treatment plan to enhance therapeutic outcomes. Furthermore, lifestyle, diet and behavioural changes may be recommended to strengthen treatment and health autonomy. As well as encouraging regular treatment and connection with community, family, and other health professionals, such as general practitioners, specialist services and psychologists.
Liebling, A. & O’Farrell, M. (2009). Auricular Acupuncture and Addiction: Mechanisms, methodology and practice. Churchill Livingston.
Stuyt, E.B., & Voyles, C.A., (2016). The National Acupuncture Detoxification Association protocol, auricular acupuncture to support patients with substance abuse and behavioural health disorders: current perspectives. Substance Abuse and
Rehabilitation, 2016 (7), 169-180.
Turning point. (n.d.). About Addiction. https://www.turningpoint.org.au/treatment/about-addiction
